Simplifying the vaccine: Why a new COVID booster each fall could be the norm moving forward
Ever since the first iteration of the COVID-19 vaccine, it seemed like no one was entirely sure how long to wait between booster shots — or exactly how many we should be getting.
Indeed, years later, all that is clear is that one series of shots is not enough. That’s because SARS-CoV-2 is not the kind of virus (nor vaccine) that provides durable — meaning, lifetime — immunity; rather, it is, like influenza, a vaccine that confers only short-term immunity. Hence, like influenza, it seems that a new vaccine for COVID-19 each year, based on newly circulating variants, is the best public health protection.
“Having vaccines is not sufficient. We need to have them be used.”
Hence, as the coronavirus has mutated over the last couple of years, vaccines have evolved. But how vaccines will be doled out in the future, and exactly when, remained unclear.
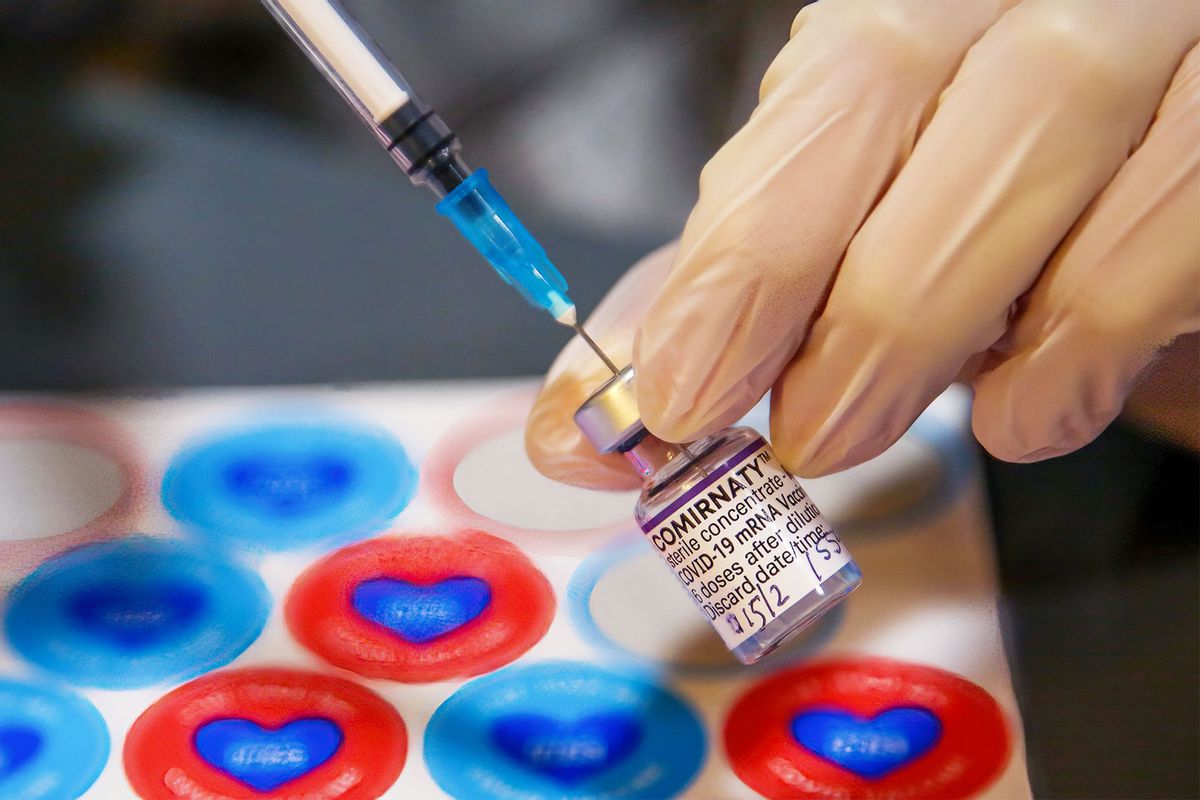
Now, we finally have some vision of the future of COVID vaccination from government public health officials. This week, the Vaccines and Related Biological Products Advisory Committee (VRBPAC), an independent advisory committee for the Food and Drug Administration (FDA), held a meeting providing insight on what an endemic COVID-19 future might look like. Specifically, the committee voted in favor of phasing out the primary two-shot series that targets the original SARS-CoV-2 strain and vaccinating individuals moving forward with the latest formulation that targets more recent subvariants.
“Speaking with colleagues, friends, family — questions I’m answering from the community,” said Archana Chatterjee, VRBPAC member and dean of the Chicago Medical School. “There’s so much confusion about these different formulations that I think anything we can do to ease up on that confusion and simplify things is going to be a good thing; having vaccines is not sufficient. We need to have them be used.”
The 21-0 vote followed a proposal released earlier this week that outlined a future where the schedule for COVID-19 shots could look like a flu shot, meaning that most people would be advised to get whatever the latest version of the vaccine is based on the strain that is most prominent and circulating that year. In the briefing document released prior to the meeting, the FDA said the proposed change would be “similar to the approach with influenza.” Under the proposal, manufacturers, the FDA and independent experts would decide which strain to target in fall by June, which is similar to the flu vaccine process each year. Researchers usually look at what’s circulating in the southern hemisphere to determine which variant to target in the annual influenza.
Want more health and science stories in your inbox? Subscribe to Salon’s weekly newsletter The Vulgar Scientist.
While members of the committee were supportive of such an approach, a vote didn’t follow.
“I think this is a reasonable approach. We have to keep reminding ourselves that this is not influenza and we need to keep paying attention to that to make sure we don’t just follow that dogma because we’re used to doing it,” said Dr. Bruce Gellin, a temporary voting member of the panel. “We’ll try this this time. I don’t think we’re setting it in stone and we’ll see how it goes. We may need to adjust along the way.”
The idea behind simplifying the coronavirus vaccine strategy is to make it less confusing.
“Because of [the coronavirus’] rapid evolution we’ve needed to adjust our approach over time, and we’re now in a reasonable place to reflect on the development of the COVID-19 vaccines to date to see if we can simplify the approach to vaccination,” said Dr. Peter Marks, FDA’s top vaccine official at the all-day meeting.
According to data from the Centers for Disease Control and Prevention, only 15 percent of the U.S. population have received the latest bivalent COVID booster.
“We can’t keep doing what we’re doing,” Gellin said. “We have to move on.”
Read more
about COVID-19 vaccines

